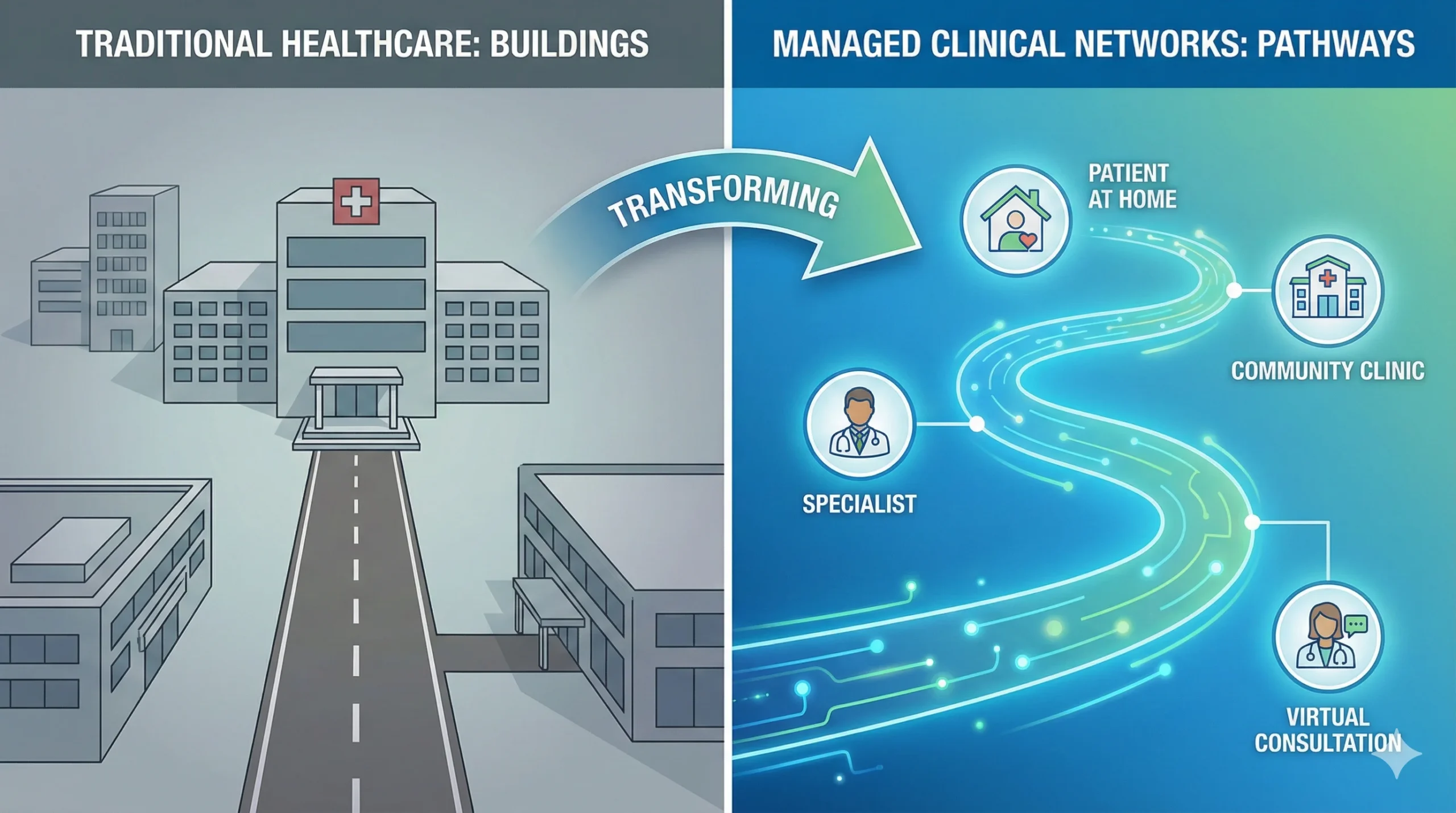
In the traditional model of healthcare, patients often feel like items on a conveyor belt that keeps stopping. They see a GP, wait months for a referral, see a specialist at a local hospital, get transferred to a city hospital for surgery, and then get discharged with little communication back to their local doctor. This fragmented system relies on buildings—hospitals and clinics—rather than the patient’s actual journey.
Managed Clinical Networks (MCNs) are the solution to this fragmentation.
An MCN is defined as a linked group of health professionals and organizations from primary, secondary, and tertiary care, working together across organizational boundaries to ensure equitable provision of high-quality services.
Unlike informal professional groups, an MCN has a formal management structure and is accountable for the delivery of care. They represent a fundamental shift in healthcare philosophy: moving from a “building-centric” model to a “patient-pathway” model.
The Core Philosophy: “Pathway over Premises”
The defining characteristic of a Managed Clinical Network is that it ignores geographical and organizational boundaries. In a standard healthcare setup, a hospital is a silo. If you live near a large teaching hospital, you might get excellent cardiac care; if you live in a rural area, you might not.
MCNs dismantle this “postcode lottery.”
By virtually linking a rural GP, a local nurse specialist, and a world-class surgeon in a distant city into one single team, the network ensures that every patient follows the same evidence-based protocol, regardless of where they enter the system.
This concept is similar to a State Wide Area Network in the IT world. Just as a SWAN connects digital infrastructure across a vast region to create a seamless flow of data, an MCN connects human expertise and clinical protocols across a region to create a seamless flow of care. The goal is the same: connectivity that makes distance irrelevant.
Anatomy of an MCN: Structure and Governance
What makes a network “managed” rather than just a social club for doctors? The answer lies in strict governance. An MCN is not a loose affiliation; it is a structured organization with clear accountability.
1. The Steering Group
The brain of the MCN is the Steering Group. This is a multidisciplinary board that meets regularly to set the strategy. Crucially, it is not just doctors. A functional Steering Group includes:
- Clinicians: Consultants, GPs, Nurses, Allied Health Professionals.
- Managers: Finance and operational leads.
- Patients: A distinct feature of MCNs is the mandatory inclusion of patient representatives to ensure the service is user-focused.
2. The Lead Clinician
Every MCN appoints a Lead Clinician. This person does not necessarily “manage” the staff in a traditional HR sense—a nurse in the network still reports to their hospital matron. However, the Lead Clinician has authority over the clinical standards. They are responsible for driving quality and ensuring protocols are followed.
3. Quality Assurance and Data
MCNs run on data. You cannot manage what you cannot measure. The network must agree on a dataset that every partner collects.
This is where performance benchmarking becomes critical. Much like an Academic Performance Indicator is used to measure and rank the output of educational institutions against standardized metrics, MCNs use clinical quality indicators to benchmark hospitals against each other. If one hospital has a higher post-operative infection rate than the rest of the network, the data highlights it immediately, allowing the MCN to intervene and offer support.
Real-World Examples of MCNs in Action
To understand the power of MCNs, we must look at specific specialties where they have revolutionized care.
Diabetes MCNs
Diabetes care requires input from dietitians, podiatrists (foot care), ophthalmologists (eye care), endocrinologists, and GPs. In the past, these were separate appointments in separate locations.
- The MCN Approach: A Diabetes MCN creates a unified IT system. When a podiatrist sees a diabetic ulcer, the specialist at the hospital can see the notes instantly. The network ensures that eye screening rates are identical across the whole region, preventing blindness through standardized preventative care.
Cardiac Networks
Time is muscle. In cardiac care, MCNs have been used to redesign the “heart attack pathway.”
- The MCN Approach: Instead of taking a heart attack patient to the nearest hospital (which might not have a catheter lab), the ambulance crew follows a network protocol to bypass local units and go straight to a specialist “Heart Attack Centre.” The MCN provides the governance structure that allows ambulance services and hospitals to agree on this bypass protocol safely.
Neonatal Networks
Babies born prematurely need different levels of care.
- The MCN Approach: The network designates “Level 1” units for basic care and “Level 3” units for intensive care. The MCN manages the transfer service, ensuring that if a baby in a small hospital gets sick, there is a dedicated team and bed ready at the specialist centre, and they are returned closer to home as soon as they stabilize.
The Major Benefits of the MCN Model
When implemented correctly, Managed Clinical Networks offer a “triple win” for the health system.
1. For the Patient (The User)
- Equitable Access: Patients get the right treatment based on need, not geography.
- Seamless Transitions: The “black hole” between the GP referral and the hospital appointment is bridged.
- Voice: Through patient representatives on the Steering Group, users have a direct line to the people making decisions.
2. For the Staff (The Provider)
- Education: MCNs run annual conferences and training days, allowing staff in smaller hospitals to learn from leading experts in tertiary centres.
- Reduced Isolation: A specialist nurse working alone in a rural clinic becomes part of a supportive regional team.
- Standardization: Staff don’t have to guess the best treatment; the network provides clear, evidence-based guidelines.
3. For the Organization (The System)
- Efficiency: By centralizing complex procedures and decentralizing routine follow-ups, resources are used better.
- Scale: MCNs have greater bargaining power when procuring equipment or negotiating for new drugs.
Challenges and Future Outlook
Despite their success, MCNs face hurdles. The biggest is funding. Because MCNs span multiple health boards or trusts, arguing over who pays for the network manager or the administrator can be contentious. Furthermore, IT interoperability remains a nightmare; getting a hospital computer to talk to a GP computer is often harder than the medicine itself.
However, the trajectory of modern healthcare is clear: integration is the future. Whether called Managed Clinical Networks, Integrated Care Systems (ICS), or Accountable Care Organizations (ACOs), the principle remains the same. The era of the isolated hospital is ending, replaced by the era of the connected, managed network.